Originally published by our sister publication Gastroenterology & Endoscopy News
A step-by-step workflow for endoscope precleaning can be applied consistently for endoscopes in different outpatient clinics, saving time and improving patient and staff safety, according to a process improvement initiative presented at the 2022 annual meeting of the Association for Professionals in Infection Control and Epidemiology.
Precleaning kits, strategic placement of hand sanitizer and rehearsing workflows in mock clinical settings decreased the amount of time required to preclean an endoscope in an outpatient sigmoidoscopy clinic by half—from almost nine minutes before the project to less than five minutes.
“This process can save time while also creating a safer work environment for both patients and staff,” said lead researcher Michell Reyes, MT, CIC, FAPIC, an infection control manager at Memorial Sloan Kettering Cancer Center (MSKCC), in New York City.
At his institution, the final workflow efficiently interlinked tasks to minimize cross-contamination. He said this type of organized, safe and efficient precleaning workflow can be easily adapted to other specialty settings.
Defining the Goal
According to Mr. Reyes, he and his team wanted to design a better workflow that would make both staff and patients feel safe, while also following regulatory recommendations.
Before the initiative, he said, procedures were performed inconsistently. Staff did not follow a clean-to-dirty workflow, which resulted in contamination of clean supplies and clean areas while increasing the risk for staff and patient exposures to potentially infectious materials.
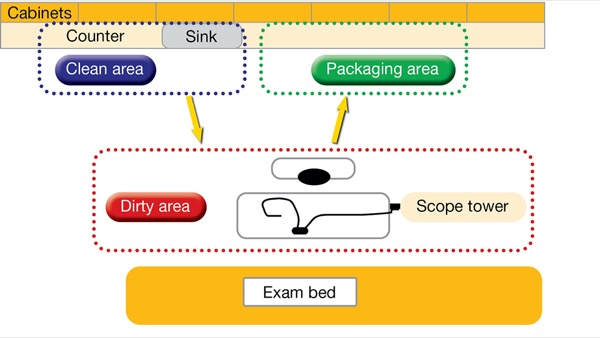
Mr. Reyes told Priority Report that he and his co-investigators set out to design a standardized, directional workflow to improve efficiency, safety and compliance with standards of care (Figures 1 and 2). They assembled a multidisciplinary team with nurses, patient care technicians, as well as support services and infection prevention staff.
Assembling a team made up of the front-line staff who are responsible for precleaning in outpatient clinics was important, he said, emphasizing the role of technicians and their invaluable contribution to the process improvement project. The technicians were able to contribute significantly to articulating barriers and suggesting realistic workflow strategies. In addition, Mr. Reyes and his co-investigators emphasized that the involvement of facility and departmental leadership also was integral to developing a solid workflow and addressing potential barriers, such as location of supplies and counter space.
“To implement a new process, we need to include the people actually doing the work on developing workflows,” Mr. Reyes said. “These workflows will fit in any clinical practices, private doctors’ offices or health centers where endoscopic procedures are done.”
Through regular progress meetings and observations held over a six-month period, the team addressed obstacles, including cross-contamination and front-line staff concerns about exposure to infectious materials due to perforated scope containers that can leak. They created detailed workflow maps outlining start-to-finish precleaning procedures that would reduce cross-contamination while keeping staff members protected.
One important obstacle identified was inconvenient location of supplies and limited counter space. But, according to Mr. Reyes, the workflow can still be implemented successfully in sites with these limitations. “This process can work if staff use portable trays or stands and organize the layout of the rooms,” he explained. “The most important factor is that staff can identify the clean area versus the dirty area.”
Implementing the Workflow
As part of the initiative, technicians rehearsed and performed the precleaning workflow in various mock clinical settings and examination room layouts to identify areas for improvement and refine any steps, when necessary.
Before implementation, related workflow tasks were separated into four distinct areas:
- Setup: The nursing staff assisted in delineating and identifying which tasks should be done in predetermined clean and dirty areas.
- Precleaning: Barriers identified during real-world observation were noted and corrected during simulation.
- Packaging: Uniform non-perforated scope containers were purchased and distributed to the entire clinic.
- Transport: Staff felt safe taking the used scope in a closed, fluid-resistant container to the soiled utility room.
Together, the multidisciplinary team was able to identify key concepts that tend to be misunderstood by staff members performing precleaning—for example, directional flow and clean versus dirty equipment.
“As a result of this systematic and organized improved initiative,” Mr. Reyes said, “the time spent precleaning decreased substantially” and safety was improved.
Creative Solutions May Be Needed
Asked to comment on the project, Amiee Mingus, RN, BSN, the vice president of clinical operations at PE GI Solutions in Jamison, Pa., agreed, emphasizing that the steps for precleaning cannot be skipped because they are an essential part of reprocessing an endoscope.
“Patient safety and infection prevention and control depend on every step being performed in a timely manner. If any step of precleaning is skipped or delayed, it can lead to bioburden buildup in the scope,” she said. “If space for performing precleaning is lacking, I’d investigate the possibility of using a rolling cart or table that can be moved around to accommodate the other necessary equipment in the room, but it may take some brainstorming to figure out how to accomplish the task in limited space.”
In addition, identifying and using proper personal protective equipment and providing hand sanitizer will continue to prevent workplace exposures for staff performing precleaning, she said.
Another key for the MSKCC team was collaboration with infection prevention staff to facilitate discussions about safety concerns. According to the project team, staff safety improved due to these conversations because safety was ultimately recognized as a top priority from leadership to front-line employees.
—Meg Barbor, MPH
Ms. Mingus and Mr. Reyes reported no relevant financial disclosures.