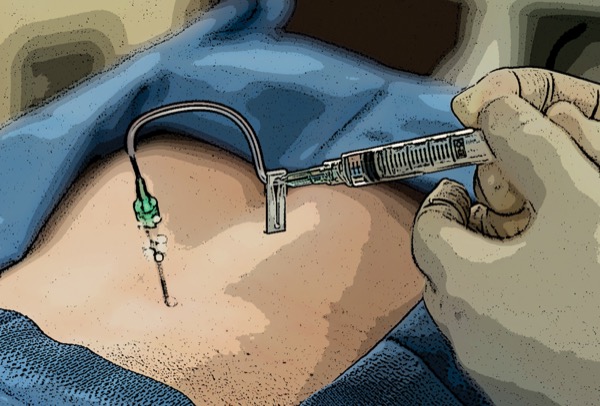
SAN FRANCISCO—One of the first studies of its kind has shed much-needed light on the reasons that medical malpractice litigation occurs in relation to epidural steroid injections.
The analysis found that neurologic injuries purportedly associated with epidural steroid injections are one of the most common reasons. Of interest, both permanent loss of function and paralysis were associated with verdicts for the plaintiff or settlement payouts.
“There was a 99% increase in the rate of epidural steroid injections administered between 2000 and 2014,” said Caleb Ting, a medical student at the University of California, Riverside. “Part of this increase, we assume, is that as our patient population gets older, it’s riskier to do surgeries, so we’re opting for more conservative measures for pain management, including epidural steroid injections.
“Although epidural steroid injection is a common procedure and complications are rare, it poses the potential for severe consequences,” he continued. “Therefore, we believe that analyzing these malpractice claims may provide insight into medicolegal risk factors, and improve delivery of care.”
The researchers queried two legal databases for relevant cases between 1998 and 2021, which yielded a total of 7,493 results. After cases were screened for relevance, they were categorized according to the type of grievance by the plaintiff.
“We only included cases where the epidural steroid injection was performed by a medical doctor and was the primary procedure,” Ting explained. “What’s more, the case had to specifically cite the epidural steroid injection as the reason for litigation.”
Presenting the study at the 2023 annual meeting of the American Society of Anesthesiologists (abstract A1071), the researchers revealed that 19 cases were specifically due to epidural steroid injection. Two cases resulted in verdicts for the plaintiff and five resulted in settlements. Cases involved physicians across five specialties, including 14 from anesthesiology, two from diagnostic radiology, and one each from physiatry, emergency medicine and orthopedic surgery. Five of the physicians were fellows trained in pain management.
Analysis of geography found that more cases were filed in California (five) than any other state, followed by New York and Texas (three each), as well as Georgia and Pennsylvania (two each). Florida, Illinois, North Carolina and Virginia had one case each. Spinal regions mentioned in the lawsuits included cervical (eight cases), thoracic (six cases) and lumbar (five cases).
The investigators assigned each case a broad category for the cause of litigation. It was found that plaintiffs alleged neurologic deficits in 12 cases, permanent and uncontrollable pain in two cases, lack of informed consent in two cases, and one case each for use of a non-standard medical device, wrongful death and incomplete patient history acquisition.
“We found that inadequate informed consent was primarily jury dependent,” Ting said. “Whereas some juries were satisfied when the chart stated that the patient had signed the consent form, other juries believed the physician was at fault when they didn’t go into detail about the complications that can arise from epidural steroid injections.”
Ting also reported that in the case of settlement or plaintiff verdict, payment amounts ranged between $75,000 and $625,000. These awards, the researchers noted, were generally lower than for other procedures related to the spine. Of the seven plaintiff verdicts, five epidural steroid injections were performed at the cervicothoracic level.
“There are three prominent messages that we took away from this research,” Ting concluded. “First, physicians performing epidural steroid injections should make it known that they adhere to current standard-of-care guidelines, whether they’re published by the pain management societies or by the ASA. It’s also important that physicians present consent forms and offer patients very comprehensive education.”
Finally, the researchers stressed the importance of proper procedure documentation. “There was one case that actually cited dictation errors to demonstrate physician irresponsibility,” he said.
For James P. Rathmell, MD, the results of the analysis were not particularly surprising.
“We have published several studies [Anesthesiology 2011;114:918-926; Anesth Analg 2019;129:255-262] that show that persistent neurologic injuries do occur with these injections, and direct needle trauma to the spinal cord or spinal nerves is the most common cause of injury,” said Rathmell, the Leroy D. Vandam Professor of Anaesthesia at Harvard Medical School, in Boston. “We have no way to get at the actual incidence, but these injuries are uncommon.”
According to Rathmell, clinicians can take several steps to protect themselves against litigation from use of epidural steroid injections.
“Precise use of image guidance for needle placement is the best way to make these injections as safe as possible,” he said. “Although discussing the possibility of nerve or spinal cord injury with patients is reasonable—mostly to reassure them that these injuries are very uncommon—informed consent does not protect against sloppy, imprecise needle placement that results in neurologic injury.”
That said, Rathmell was quick to remind his peers that simply following guidelines does not protect against neurologic injury, and cautioned that practitioners should only perform epidural steroid injections in patients who are likely to benefit from them.
“That is where the guidelines offer some help in guiding good patient selection,” he noted. “As to best practices, I go back to what I said above: Precise technique when performing epidural injections is critical, particularly when performing them at the level of the cervical spine.”
By Michael Vlessides
Rathmell and Ting reported no relevant financial disclosures.